Balancing Health Benefits and Risks of ACT Subsidies for Africa
- Rural population
- Malaria
- Subsidies
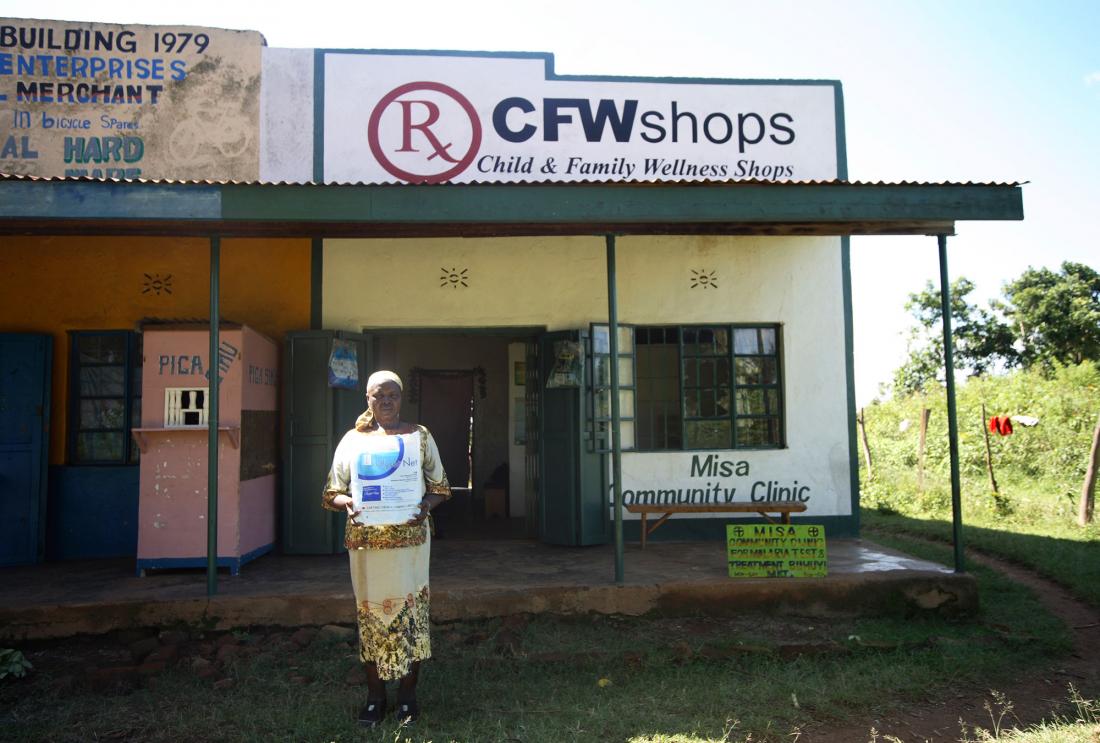
Researchers distributed vouchers for antimalarial drugs and malaria rapid diagnostic tests, redeemable at four local drug shops in Western Kenya. Taking some subsidy money away from anti-malarial drugs and putting it towards subsidizing and promoting rapid diagnostic testing could improve targeting.
Policy issue
Malaria is one of the world’s foremost public health concerns, killing over 600,000 people every year. In many malaria-endemic regions, resistance has developed to all but one class of antimalarial drugs, called artemisinin combination therapies (ACTs). ACTs sold in the retail sector are unaffordable for the poor, and although heavy subsidies can make them accessible, the benefits of treating more people and lowering transmission rates must be balanced against the risk of overtreatment, which can hasten the development of drug resistance. A new malaria testing technology, the rapid diagnostic test (RDT), has made it possible to perform malaria testing in the retail sector, but these tests are not in demand at prevailing prices. How can policymakers tailor the prices of subsidized drugs and diagnostic tests to target those truly sick with malaria and prevent those who do not need ACTs from taking them?
Context of the evaluation
In Kenya, ACTs are now the only effective class of antimalarial drugs. The incidence of malaria in Western Kenya is very high, with nearly 70 percent of households self-reporting an episode of malaria in the month before baseline. ACTs at government health centers in Kenya are nominally free, but health centers are often stocked out of medication, and the remotely-located poor often cannot afford to travel the distance to get there. Consequently, many people opt to purchase cheaper, less effective anti-malarials over-the-counter at drug shops located closer to home. The Affordable Medicines Facility for malaria (AMFm) is an initiative currently being considered by major international aid agencies in which ACTs would be heavily subsidized to first line buyers throughout Africa (the subsidy policy is currently being piloted in seven countries). But such a high subsidy could lead to overtreatment. If people who do not have malaria presumptively buy ACTs without a diagnosis, this can contribute to drug-resistance, waste subsidy money, and delay appropriate treatment for the true cause of illness. Improving diagnostic access could considerably reduce overtreatment, but there has been little research so far in this area.
Details of the intervention
The intervention took place in the districts of Busia, Mumias, and Samia in Western Kenya. Researchers distributed vouchers redeemable at four local drug shops to all households within four kilometers of four rural market centers. The households were randomly assigned to one of three groups:
| Group | Intervention description |
| Comparison: no subsidy | Households received a voucher to buy ACTs at the market price of KES 500 (about US$6.25) |
| ACT subsidy only | Households received a voucher for ACTs giving them either an 80 percent, 88 percent, or 92 percent subsidy. |
| ACT and RDT subsidy | Households received an ACT voucher as in group 2, as well as a voucher for either a free RDT, an RDT for US$0.19 (corresponding to an 85 percent subsidy), or an RDT for US$0.19 that was refundable if the test was positive and an ACT was purchased. |
In order to find out what fraction of people buying ACTs were truly malaria positive—a proxy for how well the ACT subsidy under the AMFm would be targeted—the researchers also selected a random subset of the households in all treatment groups to receive the offer of a “surprise” free RDT after they completed their transaction at the drug shop.
Trained study officers were posted at each of the four participating drug shops during opening hours every day throughout the study period. When a household member came into a drug shop to redeem his or her voucher, study officers recorded details such as medicines bought, symptoms, patient characteristics, and true malaria status in case an RDT was administered.
Results and policy lessons
Under the subsidy, more people sought care for malaria. Specifically, the number of households not seeking any care decreased by 38 percent for those who received the 80 percent subsidy. The subsidy also increased the likelihood that an illness was treated with an ACT by 18 percentage points for the 80 percent subsidy, 16 percentage points for the 88 percent subsidy, and 23 percentage points for the 92 percent subsidy from 19 percent in the comparison group.
The subsidy increased access among sick children, for whom malaria is particularly dangerous. The subsidy increased the share of ill children treated with ACTs, particularly in the poorest households, and overtreatment was rare: 79 percent of children under age 14 for whom subsidized ACTs at 92 percent subsidy level were purchased tested positive for malaria. However, the subsidy led to a high rate of overtreatment among adults. Only 21 percent of adults (aged 14 and over) who took a subsidized ACT at 92 percent subsidy level actually tested positive for malaria, which leaves room for improvement in targeting the subsidy.
A slightly lower subsidy level improved targeting without significantly compromising overall access to ACTs. At the two lower subsidy levels (80 and 88 percent), households were less likely to use an ACT voucher for adults than at the AMFm target of 92 percent, but the use of vouchers for young children, who are more likely to have malaria and for whom malaria is most dangerous, was unchanged. On the other hand, while households were very willing to take RDTs, the RDT subsidy was only somewhat effective at reducing over-treatment and thus improving targeting. This was likely caused by high noncompliance - among patients over the age of 5 who tested negative, 49 percent still purchased an ACT.
While these results suggest that a slightly lower ACT subsidy than the one proposed by the AMFm would improve targeting without compromising access, the results also make it clear that a large ACT subsidy is needed in order to increase access among the neediest. Taking some of the planned ACT subsidy money away from ACTs and putting it towards subsidizing and promoting RDTs could improve targeting and be particularly effective among adults, especially if adherence to test results can be improved.

