Conditional Cash Transfers and HIV/AIDS Prevention in Malawi
- Adults
- HIV/AIDS
- Sexual and reproductive health
- Cash transfers
- Preventive health
- Conditional cash transfers
- Monetary incentives
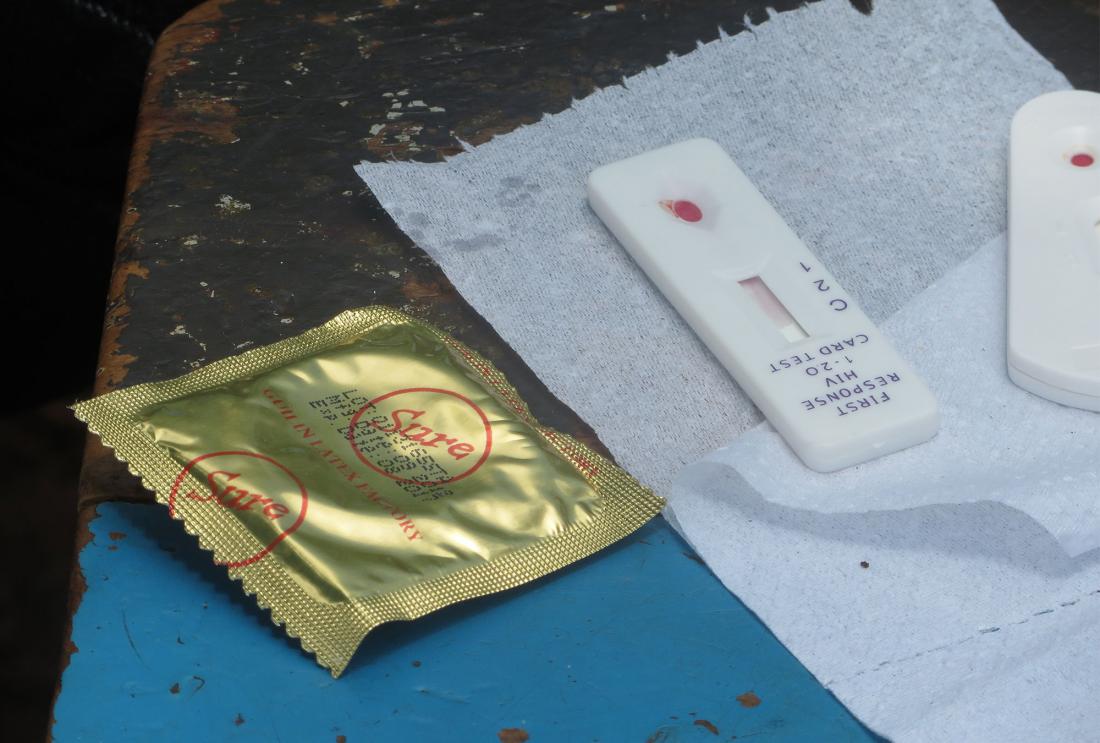
Given the extent of the HIV/AIDS epidemic, policymakers face an urgent need to develop effective treatment and prevention programs. Researchers evaluated whether offering individuals financial incentives to maintain their HIV-negative status could be an effective HIV prevention strategy in rural Malawi. The conditional cash transfer had no effect on HIV status or on self-reported sexual behavior. The receipt of the cash incentive actually increased the likelihood of risky sex among men but decreased risky sex among women.
Policy issue
At the end of 2009, more than 33 million people were living with HIV.1 Given the extent of the HIV/AIDS epidemic, policymakers face an urgent need to develop effective treatment and prevention programs. While most HIV prevention strategies target behavior change, evidence of the impact of these programs remains controversial and no single intervention has emerged as an established approach. Conditional cash transfers (CCTs) have been used successfully in a variety of settings as a means of incentivizing socially desirable behavior change, such as school enrollment or attendance at preventive healthcare check-ups. There is some evidence that CCTs could be used to prevent the spread of HIV by incentivizing individuals to stay free of sexually transmitted diseases, however more evidence is needed to understand responses across various contexts and populations.
Context of the evaluation
Eleven percent of adults in Malawi are infected with HIV/AIDS, giving the country the 9th highest prevalence in the world. Although the HIV prevalence rate in the sample area was considerably lower than the national rate, at 6.3 percent, it was comparable to, or greater than, the prevalence rate in much of sub-Saharan Africa. For comparison, in 2009, the HIV prevalence rate in Kenya and Sierra Leone was 6.3 percent and 1.6 percent, respectively. Existing research suggests that CCTs may be an effective method to reduce sexual behavior and prevent HIV. In Tanzania, a program that offered cash incentives for remaining free of curable sexual transmitted infection (STIs) led to a significant reduction in STI infections when participants were offered a large transfer (US$20). However, the program had little impact when participants were offered a moderate transfer (US$10). A second study in Malawi offered girls and their parents US$15 each month to attend school, in addition to covering all school fees. After one year, girls offered the unconditional incentives were significantly less likely to be infected with HIV.2
Details of the intervention
Researchers sought to evaluate whether offering individuals financial incentives to maintain their HIV status could be an effective HIV prevention strategy in rural Malawi. Researchers measured the impact of conditional cash transfers (CCTs) on reported sexual activity, condom use, and incidences of HIV infection. The CCT program builds upon a previous evaluation of the Malawi Diffusion and Ideational Change Project (MDICP), where respondents were offered free door-to-door HIV testing and randomly assigned cash incentives to obtain their results from nearby testing centers.
Among MDICP participants that agreed to be tested for HIV in 2006, 1,307 were randomly invited to participate in the CCT program. Seventy-six percent of the sample enrolled as individuals, while the remaining enrolled as couples. Participants were offered incentives of random amounts ranging from zero to 2,000 MWK (approximately US$16) for individuals, and from zero to 4,000 MWK (approximately US$32) for couples, all of which were conditional on maintaining their HIV status for approximately one year. The incentives represented a significant amount of money for respondents, with the higher amount equal to approximately three to four months wages.
Throughout the year, program staff visited participants in their homes and asked about their sexual behavior in the last nine days through interview-administered sexual diaries. From these diaries, researchers developed several indicators of risky or safe sexual behavior, including pregnancy, incidents of vaginal sex, number of days having vaginal sex, condom usage, and the presence of condoms at home. Data was collected three times over the period of the study, at roughly three-month intervals. After the last round of surveys, a trained nurse visited each participant to test for HIV, and financial incentives were awarded based on whether they had maintained their HIV status. Approximately one week later, each respondent was surveyed again about his/her sexual behavior in the past week.
Individuals who were HIV-positive at the start of the program automatically received the monetary incentive at the end of the study. These individuals were included in the sample to avoid the possibility that being excluded from the study would signal their HIV positive status to outsiders.
Results and policy lessons
The promise of financial incentives of any amount had no effect on subsequent self-reported sexual behavior or HIV status. Self-reports may be biased towards individuals over-reporting safe sexual behavior, particularly for individuals receiving higher incentives. Despite these potential biases, which would lead to an overestimation of program impact, financial incentives appear to have had no effect.
Although the conditional offer of money had no impact, receiving cash after the final round of HIV testing was found to have large effects on respondents' self-reported behavior. In the week following the receipt of the cash transfer, men who received the money were 12.3 percentage points more likely to have had vaginal sex and had approximately 0.5 more days of sex. While self-reported condom use among these men increased by 6.9 percentage points, overall, they were 9 percentage points more likely to engage in riskier sex. Women, on the other hand, were 6.7 percentage points less likely to report engagement in risky sex, a result that is driven by abstinence rather than increased condom use.
These results provide evidence that money given in the present may have much stronger effects than rewards in the future. Unlike the CCT program in Tanzania, this study found no effect of financial incentives on risky sexual behavior, suggesting that policymakers should use caution in considering CCTs as a tool for HIV prevention. The fact that a cash grant reduced risky sexual behavior for women provides further evidence that money can be protective for women, but cautions that programs that aim to motivate safe sexual behavior in Africa may be sensitive to the local and/or cultural context, and the degree of agency individuals to determine their own sexual behaviors.
